Abstract
Cytokine release syndrome (CRS), central nervous system (CNS) abnormalities and B-cell aplasia have been widely reported in recent clinical trials for chimeric antigen receptor T-cell (CAR-T) therapy. In our study, we also note that patients who received CAR-T therapy were easily to develop coagulopathy, even disseminated intravascular coagulation (DIC), which increased the risk of treatment related mortality (TRM) and required timely intervention. Therefore, it is important to pay attention to the symptom and find out the way to improve it.
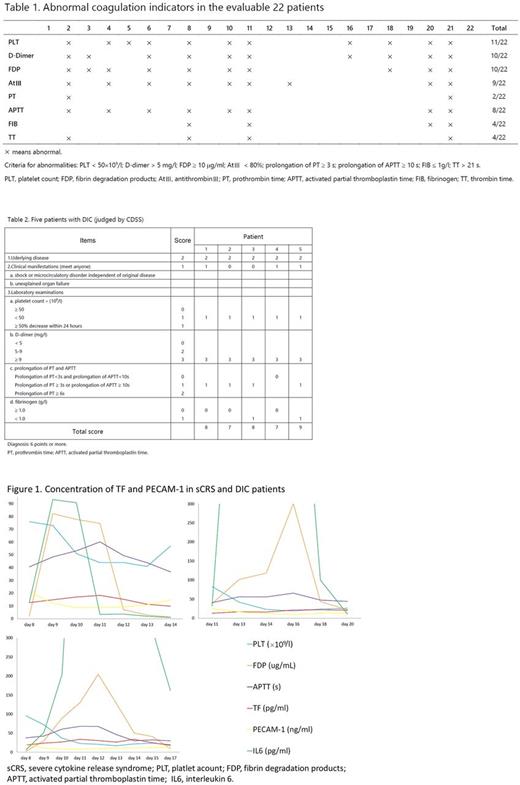
In our phase-1 clinical trial (NCT02965092) for B-cell acute lymphoblastic leukemia (B-ALL), we dynamically monitored the coagulation indicators and treated coagulopathy. Twenty-five patients (median age 28, [10-61]) were recruited into the trial and they underwent leukapheresis on day -11. Then they were subjected to the lymphodepleting regimens (fludarabine + cyclophosphamide, n=22; fludarabine, n=2; cyclophosphamide, n=1) on day -7~-5. Finally, they received the infusions of anti-CD19 CAR-T cells at a median dose of 4.5×106/kg (3.2-8.3×106/kg) on day 0~2. Excluding 3 patients who quitted from the trial for rapid progression of disease, and 3 patients who have not reached one-month follow-up time point yet, the overall one-month response rate for the evaluable 22 patients was 86.36%. Up to date, the longest leukemia free survival (LFS) was 16 months (median 5 months, [1-16]). As for side effects, 12 patients developed grade 2-3 CRS, 2 patients suffered from CNS symptoms, and no patients experienced serious infections. Besides, the obvious coagulopathy caught our attention. Eleven patients (11/22, 50%) developed coagulation dysfunction, manifested as petechiae and abnormal laboratory indicators (Table 1), such as deceased platelet count and fibrinogen, increased D-Dimer and fibrin degradation products, prolongations of activated partial thromboplastin time, prothrombin time and thrombin time. According to Chinese DIC Scoring System (CDSS), 5 of these 11 patients should be diagnosed as DIC (Table 2).
Furthermore, we collected patients' plasma to measure the concentrations of tissue factor (TF) and platelet endothelial cell adhesion molecular-1 (PECAM-1), which are 2 vascular endothelial molecules that may play important roles in inflammation and coagulation. It was observed that coagulation disorders were more common in patients who developed severe CRS. Here we present the experiment results of 3 patients who experienced severe CRS and DIC at the same time. As shown in Figure 1, when the concentration of interleukin 6 rose and indicated CRS, the coagulopathy happened. At the same time, the TF concentration rose and PECAM-1 concentration dropped. Taken together, these data indicate that there is a relationship between CRS and DIC. We hypothesize that the cytokines released from inflammatory cells during CRS could cause dysfunction of endothelial cells and destroy the integrity of endothelial barrier, thus resulting in coagulopathy. However, the mechanism remains poorly understood, more in vivo experiments should be conducted to identify the mechanism, which may suggest novel therapeutic targets for coagulopathy.
In conclusion, our data demonstrate that coagulation disorders are common side effects in CAR-T therapy, and suggest that TF and PECAM-1 are critical parameters in the pathogenesis of CRS-related coagulopathy. Investigators should pay more attention to coagulopathy and take preventive measures to avoid DIC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.